Blog
Aging Parents, Adult Children: Subject of YouTube Drama
There’s a new dramatic series on aging parents and their adult children on YouTube. These brief vignettes, with 13 episodes in all, capture issues facing families as parents become less able to care for themselves and their children try to intervene/help. I saw the first one and thought it was very powerful.
Here’s a link to what Paula Span, of the New Old Age blog at the New York Times has to say about it: Drama of Aging and Caregiving, on YouTube
Here’s the first episode:
Gay Seniors: Diversity Training for LTC Staff
Maybe it’s because I live in the New York metropolitan area, but it seems every nursing home I’ve worked in is filled with residents and staff from all over the world. I find it an exciting environment with the opportunity to learn about different cultures at every turn. Somehow, despite our differences, we make it work and provide top-notch care for our residents. Unless they’re gay. Or lesbian, bisexual, or transgendered (LGBT). Then many LGBT residents, no matter what country they hail from, feel they need to go back into the closet and hide who they are from those caring for them. They fear the prejudice of staff members and rightly so, based on a number of conversations I’ve had with co-workers about the issue. According to The Aging and Health Report released by The National LGBT Health and Aging Center, 21% of LGBT seniors do not disclose their sexual or gender identity to their physician. Their physician.
If you’re looking for resources to address LGBT issues in LTC, consider showing your staff the award-winning hour-long documentary Gen Silent or using one of their training programs. I had the opportunity to view the film at the American Psychological Association conference last month and think it would make an excellent tool for addressing sexual diversity. Given the strong feelings many staff members have on homosexuality, a training program is likely to be more helpful than an open discussion of the issues. As a psychologist privy to the private concerns of residents, I can tell you that you do have LGBT residents within your facilities — you just might not know who they are.

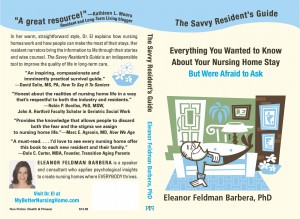
The Savvy Resident’s Guide is Now Available on Amazon.com!
I’m pleased to announce that The Savvy Resident’s Guide: Everything You Wanted to Know About Your Nursing Home Stay But Were Afraid to Ask is now available on Amazon.com!
It’s been my lifelong wish to publish a book, so I’m excited and couldn’t wait for the official book launch to tell you about it. If you think The Savvy Resident’s Guide might be useful for someone you know, please spread the word. Many thanks to all of you who helped me reach this point and thanks in advance to those of you who offer the book to those who need it.
About The Savvy Resident’s Guide:
The Savvy Resident’s Guide explains how nursing homes work and how people can make the most of their stays. This large-print guide is the only book available that is directed specifically toward residents. Its calm, pragmatic approach will reassure readers and give them practical tools for handling a nursing home stay.
Families will find answers to many of their own questions about nursing homes in The Savvy Resident’s Guide. Reading the stories of the resident narrators will help family members understand what Mom or Dad worries about after they’ve left for the day.
Staff can use The Guide as a helpful adjunct to their work since it answers questions without requiring staff time. It’s a ready reference book that makes an ideal addition to the admissions package.
Students of many disciplines — nursing, psychology, social work, rehab, medicine, etc. — will benefit from this overview of life in long-term care. They’ll gain insight into the typical concerns of nursing home residents and absorb a person-centered approach to managing these concerns.
For more information and to order the book, visit The Savvy Resident’s Guide: Everything You Wanted to Know About Your Nursing Home Stay But Were Afraid to Ask
Me, with my first proof of The Savvy Resident’s Guide!
The second (and hopefully last) proof is on its way.
The Savvy Resident’s Guide: Everything You Wanted to Know About Your Nursing Home Stay But Were Afraid to Ask will be available soon!

5 Reasons to Educate Residents About Their Illnesses (LTL mag online)

Here’s my latest article in Long-Term Living Magazine online:
5 reasons to educate residents about their illnesses
“How long have you had Parkinson’s?” the psychologist asked Mr. Jones during his initial evaluation.
“They just told me the diagnosis when I got here last week, but I suppose I’ve had it for a while.” He said it casually, but his hands were clenched and his voice held a note of tension.
“Did the doctor explain what it is or give you information about the Parkinson’s Foundation?”
“No. All I know is that it’s the same disease that young actor has—what’s his name?”
“Michael J. Fox.”
“Yeah, that’s the one.”
The psychologist assured the resident she’d bring him a pamphlet from the Parkinson’s Foundation the following week. It would work better, she thought to herself, if the medical staff provided the physical health information so she could follow up with the mental health aspects.
Residents often enter long-term care with surprisingly little knowledge about their conditions, whether they have a recent diagnosis or have been living with an illness for many years. This lack of information isn’t good for residents, families or facility staff.
Here are five reasons why we should teach our residents about the illnesses they live with:
1. Education leads to more active resident involvement in care.
When residents have information about their illnesses, they are more able to accurately report their symptoms to the medical team and to provide the type of information that improves treatment. A resident without knowledge is a passive recipient of medication and care; a resident with knowledge can partner with his or her medical team to address needs and find effective solutions. Joan, for instance, had multiple sclerosis and was keenly aware that the hot summer made it difficult for her to walk in rehab. She was able to work with her therapist to find more manageable activities so that she could continue with her rehab program during the summer months. Contrast this with Leon, who blamed himself for his MS symptoms, believed his difficulty walking was a personal failure, and was referred for psychotherapy when he stopped attending rehab. With encouragement and some psychoeducation about his illness, Leon was literally able to get back on his feet again.
2. Knowledge increases compliance.
Uneducated individuals are less likely to comply with treatment recommendations or may reject medications due to side effects without fully considering potential benefits. Individuals who understand why particular medications are given and how to cope with potential side effects are more likely to comply with treatment. They’re also more likely to have reasonable, informed objections for foregoing a particular course of treatment—reasons that can be readily understood and documented. For example, Lucille was initially resistant to the dialysis treatments that were recommended for her. Once she gathered information and spoke to some other residents in the dialysis program, she ultimately decided that its life-saving benefits were worth the time and discomfort of the treatments. Thomas, on the other hand, decided against dialysis and was able to explain and document his end-of-life wishes clearly, based on his knowledge of his illness.
3. Information reduces anxiety.
For more, visit Long-Term Living Magazine online: 5 reasons to educate residents about their illnesses

See you in September! (Dr. El takes a break)

Hello, Folks! Summer is my favorite season and I’m going to take a little blog break and enjoy the rest of it. I’ll be back the week of September 10th (unless I can’t contain myself).
Meanwhile, here’s an interesting article on end-of-life family reconciliation by Marc Agronin, MD: Struggling With an Abusive Aging Parent
And here’s a little comment on gratitude by one of my residents:
Florence: “I thank God for every day.” She smiled at me. “I might not remember what day it is, but I thank him for it anyway.”

Social Media in Health Care: Focus of APA Talk
Last weekend I was in Orlando, Florida for the American Psychological Association conference, where I spoke as part of a symposium on Social Media in Long-Term Care Settings. We discussed concerns around maintaining privacy and confidentiality, as well as the use of social media to improve care. Of course, I talked about my blog, how it developed, recommendations for those considering beginning their own blogs, and ways in which I’ve used my blog for therapeutic purposes with the residents. Below you can see me with co-presenters, Drs. Keely Kolmes, Geoff Lane, Mary Lewis, and Pat Bach, who are all psychologists experienced in the use of social media in health care.


New Old Age column: More Older People Treated for Depression

The New York Times New Old Age blog has an interesting, hopeful article by Paula Span regarding treatment for depression in older adults. Regarding the stigma of psychotherapy the article mentions, I’ve found nursing home residents to be very receptive to my visits, especially when I phrase my help as “extra support during a stressful time.” Everyone agrees that entering a nursing home is stressful. (See my earlier post, The Stress of Nursing Home Admission, for more on this.) Occasionally, when someone is resistant but I can tell they need me, we postpone the decision to officially start psychological services and I tell them I’ll “just stop by next week to see how things are going.” Nine times out of ten, they’re glad to see me and appreciative that I showed up when I said I would.
Here’s the start to the New Old Age post; click on the title below to read the whole article:
More Older People Treated for Depression
By PAULA SPANAnna Hill’s mother-in-law had suffered from depression for years, it was clear in hindsight, and had denied it for years, too. Only 73, she’d lost interest in doing much of anything. In chronic pain after an earlier accident, she was taking high doses of methadone. Last November, she stunned her family by declining, at the eleventh hour, to come to Thanksgiving dinner.
“I’d only seen her in a nightgown for a year straight,” said Ms. Hill, 42, an accountant in Atlanta. “She was just rotting away in bed, watching TV and taking methadone.”
Depression in the elderly is a mixed picture these days.
For years, mental health specialists lamented that depression was seriously underdiagnosed and undertreated in the elderly. Laypeople saw it not as a disease but as an inevitable part of aging. Doctors missed it because depression didn’t always look the way it did in younger patients — less sadness and weepiness, more physical symptoms and disengagement. Older people themselves often rejected help because mental illness carried a stigma.
In primary care practices, Dr. Jürgen Unützer and colleagues found in a large study published in 2000, only 12 to 25 percent of older people with probable depression were getting a diagnosis and being treated.
Not anymore. Over the past decade, “we’ve seen a really big increase in the recognition of depression and the initiation of treatment,” said Dr. Unützer, a geriatric psychiatrist now at the University of Washington.
For more, click on title of article above.

Falls in Older People? Anxiety Could Be A Cause
 It was previously thought that seniors who are anxious about falling tend to avoid activities that could lead to falls, thus becoming de-conditioned and increasing fall risk. New research, however, suggests that anxiety about falling itself can increase fall risk. Hadjistavropoulos, T. et al. asked older adults to walk either in a low anxiety situation (on the floor) or a high anxiety situation (on an elevated platform). Those who were more anxious (measured through heart rate, self-report, etc) had a less stable gait. In addition, those who were multi-tasking by carrying a tray had a less stable gait. The self-report of anxiety about walking was predictive of balance performance — in other words, if they said they were nervous about falling, they didn’t walk as well.
It was previously thought that seniors who are anxious about falling tend to avoid activities that could lead to falls, thus becoming de-conditioned and increasing fall risk. New research, however, suggests that anxiety about falling itself can increase fall risk. Hadjistavropoulos, T. et al. asked older adults to walk either in a low anxiety situation (on the floor) or a high anxiety situation (on an elevated platform). Those who were more anxious (measured through heart rate, self-report, etc) had a less stable gait. In addition, those who were multi-tasking by carrying a tray had a less stable gait. The self-report of anxiety about walking was predictive of balance performance — in other words, if they said they were nervous about falling, they didn’t walk as well.
What does this mean for those of us working in LTC?
- We might consider formally or informally assessing the anxiety level of residents regarding their ability to walk.
- If residents appear anxious or report anxiety about falling, rehab therapists could discuss this with them or refer them for psychological services to address the issue. I frequently talk with residents about the circumstances around their falls and ways to avoid a repeat of the mishap, helping them to feel more in control and reducing anxiety.
- We can advise residents to focus on moving safely about their rooms (or homes upon discharge), rather than on carrying objects from one point to another.

Team Communication: A Shout-Out for CNAs

“How in the world am I going to chart this?” I wondered as I sat across from Nell, who filled her large wheelchair to overflowing. This was our second attempt at psychotherapy, which I’d discontinued a few months ago because I felt all my efforts had gone nowhere. Nell sat in her room all day, doing nothing and talking to no one, yet she was clear in her thinking and clearly depressed. She resisted all of my suggestions, recommendations, cajoling, begging, humor, and coordination with the team to adjust her medications. Efforts to connect her with her estranged family had produced a tepid response. “She’s been this way all her life,” her son told me when I’d finally called to tell him I’d stopped seeing his mom. “I’ve given up,” he added.
Now here I was, three sessions after the team had referred her for psychological services again, trying to determine a treatment strategy in the face of her extreme hopelessness.
“There’s nothing I can do,” she said, “because I can’t see.”
Her talking clock, talking watch, talking books, radio, and TV sat unused after her initial training in how to operate them.
__________________
I consulted with colleagues the next week and they encouraged me to keep going. “You’re the only person she talks to,” they said. “That has value.”
__________________
A couple of weeks later I ran into Nell’s aide in the elevator after I’d finished a staff training.
“You know she asks for you all the time, don’t you?” she said.
“She does?” I was shocked.
“You’re Eleanor, right?”
“Yes.”
“She calls ‘Eleanor, Eleanor, Eleanor’ all day long. And when she doesn’t want to take a shower, we tell her ‘Eleanor wants you to do it’ and then she goes along with it.”
“I had no idea! Thank you for telling me that.” I was flabbergasted — and relieved that my documentation could reflect some actual purpose and progress.
___________________
The next week I sat across from Nell with a lighter spirit.
“There’s nothing I can do,” she said, “now that I’ve lost my eyesight.”
“That must be a huge loss for you,” I replied.