Blog

Enhancing quality of care through design
Here’s my latest article on McKnight’s Long-Term Care News:
Enhancing quality of care through design
Last week, I attended an accessible design symposium at the Cooper Hewitt Museum in New York City to see what ideas I could use with elders in long-term care. Through listening to the symposium speakers, reading descriptions of works featured in the student design contest and viewing the Access+Ability exhibit, I found more than I had expected.
Crash course in accessible design
I suspect I’m not the only McKnight’s reader with a lack of knowledge about accessible design — even though we work with elders with abilities that are typically different than those of younger adults.
Patricia Moore, introduced as “the mother of universal design,” told the audience that her elderly grandparents inspired her work. They struggled to maintain their independence in a world that made it difficult for them. “Grandma wasn’t broken,” she said. “The tools we gave her were inadequate.”
In my crash course in accessibility, I learned that objects can be designed in ways that increase the mismatch between our bodies and the environment or, in accessible design, to intentionally decrease that mismatch. For example, the standard design of a walking cane allows it to fall to the floor, making it difficult to retrieve for someone with mobility problems. In the Cooper Hewitt exhibit, I saw canes that stayed upright when not in use.
Another speaker discussed how “designing for disability” very often results in products that are good for everyone, such as books on tape, height adjustable desks or ramps for building access that are used by parents pushing strollers and travelers with rolling suitcases, in addition to those with walkers or wheelchairs.
Nothing about us without us
There was a small, vocal group of disability activists present. When I entered the symposium I was handed a card from their organization that read, “Nothing about us … without us.” They echoed the sentiment of the speakers that increasing the diversity of people designing products and systems results in products and systems that work better for a larger number of people.
Including elders and direct care staff in more of the decisions that affect them within our organizations is likely to result in better decisions.
For the entire article, visit:
Enhancing quality of care through design

Jeweled Hearing Aids

Help in your backyard
Here’s my latest article on McKnight’s Long-Term Care News:
Help in your backyard
Amy Gotwals, the Chief of Public Policy and External Affairs at the National Association of Area Agencies on Aging, kicked off the 28th Annual Aging Conference in New York City last week, held at the New York Academy of Medicine and filled with attendees providing community-based care for elders. Her rousing keynote outlined the vast care demands of the growing wave of elders and the importance of building healthcare partnerships.
Some of Gotwals’ statistics were startling despite knowledge of the impending “silver tsunami.” Some areas of the country are projected to see an increase in Alzheimer’s diagnoses of 50% to 80% by 2025. Family caregivers between 65 and 74 years old provide more than 30 hours of care per week; for those 75 and older, it’s more than 34 hours each week.
Statistics such as these point to ways in which long-term care organizations can position themselves to be relevant far into the future by offering, for instance, memory or respite care.
Gotwals reported that local Area Agencies on Aging (AAAs), of which there are 622 across the country, are increasingly contracting with healthcare organizations to provide services such as care transitions, nutritional services, home evaluations and evidence-based self-management for chronic diseases.
In one example, San Francisco’s Institute on Aging (IOA) partnered with a nonprofit, community-based housing agency and contracted with the Health Plan of San Mateo County to provide care management services that reduced monthly spending per member by nearly 50%.
While local organizations may not be as seasoned in business promotion, they’re experts in the needs of the local community and their established presence in the neighborhood can be a boon to long-term care organizations seeking to create new partnerships.
ElderTech
After hearing Gotwals’ opening remarks, I chose a breakout session on technology and design presented by Tom Kamber, Ph.D., founder and director of Older Adults Technology Services (OATS). His is a national organization that provides technology-based senior centers and collaborates with a wide range of institutions to address the tech needs of elders.
For the entire article, visit: Help in your backyard


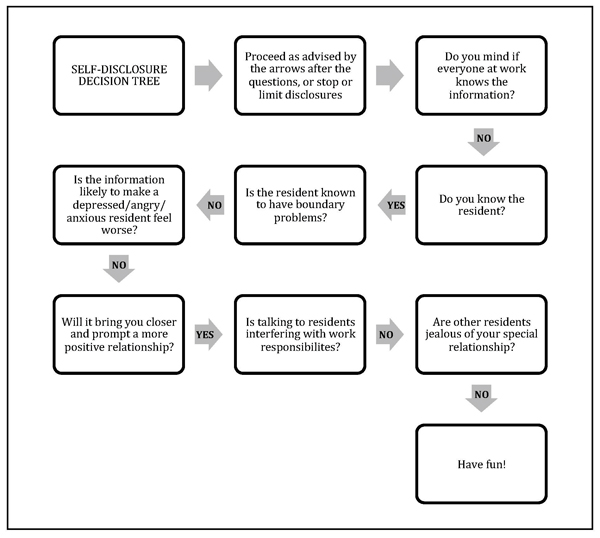
Self-disclosure: What your staff needs to know about revealing personal information to residents
Here’s my latest article on McKnight’s Long-Term Care News:
Self-disclosure: What your staff needs to know about revealing personal information to residents
As “Eileen” suggested in the comments section of a recent “Dr. El” blog, disclosing personal information can be a good way to establish a more intimate connection with residents. While self-disclosure can create warmer relationships, there also can be unintended and unwanted consequences to revealing such details.
In contrast to psychologists who study interpersonal interactions for a living, staff members are unlikely to have fully considered the impact of their self-disclosures. Doing so can improve their relationships with residents and avoid unanticipated pitfalls.
Here’s a guide* to the ups and downs of self-disclosure along with a handy flow chart (see below) to help you and your team decide when it’s the right move in any given situation. My inclination toward privacy is reflected in the flow chart, so consider it a starting point for discussion among team members or in a staff training session.
The ups
Part of the pleasure in working with elders is hearing about their lives and learning from their experiences. Sometimes revealing a detail or two from our own lives can help a reticent resident open up.
Self-disclosure allows workers to be more open and relaxed at work and to establish deeper relationships with those in their care.
Being “real” with residents can reduce the somewhat artificial boundaries between people in different phases and roles in their lives and can be part of a healthy organizational culture.
The downs
On the other hand, self-disclosure can sometimes get workers in trouble.
For the entire article, visit:
Self-disclosure: What your staff needs to know about revealing personal information to residents

4 ways to revamp work culture in the new year
Here’s my latest article on McKnight’s Long-Term Care News:
4 ways to revamp work culture in the new year
Ahhh. A new year. It’s time for a fresh start, the chance to take life in a different direction.
Many of my friends have remarked to me that they want more focus on family and friends this year. They’d like to achieve a better balance between work and home.
On the job in long-term care, perhaps the goal is to tackle the staff turnover problem or increase profitability. Or maybe the hope is that resident, staff and family satisfaction ratings will be better in 2018 or that this might be the year to achieve a five-star rating.
The common thread between these goals is deepening the attention paid to the people in our personal and business lives.
When staff members don’t feel valued, or inspired by the mission of the company, turnover increases, making it virtually impossible to have high satisfaction scores and five-star ratings. Repeatedly recruiting and training new staff cuts into profit margins and damages worker morale.
To turn things around in one’s personal life, conscious decisions can be made around limiting time on electronics or choosing to fill the new calendar year with events that connect loved ones. At work, changes can occur by prioritizing the way staff members are treated and revamping the culture of the company, altering the way people interact.
Whatever our roles in LTC, there are steps each of us can take to enhance the way we treat each other and to have a positive impact on workplace culture.
• Reevaluate mission and culture. Readers in a position to revise the organizational customs as a whole might enlist experienced guides in the process. A consulting and coaching company such as Drive, with which I’m affiliated, evaluates the strengths and weaknesses of a healthcare organization and provides ongoing support to meet goals throughout the culture change process. As a Drive team member notes in this article onCreating and Sustaining a Strong Culture, follow-through is essential. A consulting team can ensure that bumps in the road don’t become dead ends.
• Investigate known culture change programs. Thankfully, there are many people in our field who have undertaken the daunting task of creating a more gratifying long-term care environment while still following regulations. The new year is an excellent time to take a class with the Pioneer Network or the Eden Alternative, or to learn more about The Green House Model at their 1/9 webinar.
• Promote kindness. If your job in long-term care doesn’t allow you the opportunity to change the overall organizational framework, you can still be an important influence on others with whom you interact by focusing on kindness.
For the entire article, visit 4 ways to revamp work culture in the new year


People in LTC who’ve inspired me in 2017
Here’s my latest article on McKnight’s Long-Term Care News:
People in LTC who’ve inspired me in 2017
From the 102-year-old Hulk Hogan fan to the doting, selfless caregivers doing behind-the-scenes work, there are numerous people in long-term care who inspired me this year.
Take, for example:
• The 102-year-old man, still remarkably handsome, whose favorite sport is professional wrestling and who recalls fondly the days of Hulk Hogan.
• The personal companion I encountered dusting the framed family photos on the windowsill while the blind woman she cared for was taking a nap.
• The new assistant administrator who stopped me in the hallway to introduce himself and who seemed genuinely interested in my response.
• The nurses who immediately come up with a solution to a resident’s problem and then follow through with it. (“If he wants to be down at rehab early, we’ll have the night shift get him up before they leave.”) Hallelujah!
• The housekeeper dedicated to controlling infection even though it’s been a tough year for her personally.
• The legally blind 90-year-old woman who avidly follows the news and the music scene and has a strong opinion on everything. That Gaga is great, she says. The president is not.
For the entire article, visit: People in LTC who’ve inspired me in 2017


Elder love
Here’s my latest article on McKnight’s Long-Term Care News:
Elder love
I lost one of my two mothers-in-law last Monday, five weeks after she was diagnosed with pancreatic cancer. We had expected Audrey to reach 100 years of age, like her mother, but she died shortly after her 91st birthday, having spent her 90th year traveling and doing water aerobics three times a week.
Audrey had filled a hole in my life left after the death of my beloved great-aunt many years ago. Whenever I phoned my MIL, she’d answered the phone with a chipper, “Oh hello, Darling!” Emails began with the salutation, “Dear Heart,” before launching into the latest goings-on at the CCRC where she was the head of several resident programs.
After her diagnosis, she enlisted peers to take over her responsibilities, giving them her notes and training them as if they were new employees. She considered beginning a program at the care center during her brief stay, “Can you believe they don’t recycle here? I’m going to make some calls and see if we can get that started.”
She spent her last weeks shipping sentimental items to various relatives and, when she became too weak, she began instructing her sons to do the same. A steady stream of family members and friends came to say goodbye to her as she sat in her bedside chair with her makeup on and a scarf neatly tied around her neck.
It was exactly the way I’d want to go if I could have my choice.
In the days after she died, I phoned her sons and notified family members on our side of the family. I called a few of my friends and tried to get extra sleep. I confirmed my parents’ upcoming lunch invitation. I spent quality time with the cat, and with my family. I ate some chocolate.
For the entire article, visit: Elder love


Home, small home
Here’s my latest article on McKnight’s Long-Term Care News:
Home, small home
In 2014, I wrote, “I finally visit a Green House (and it blows my mind).” The Green House is designed with a spacious common area, private bedrooms and showers, unobtrusive medical items and universal workers practicing person-centered care. The model shows that it’s possible to make dramatic lifestyle improvements in long-term care.
It seemed that Green Houses were the answer, if only there weren’t so many traditional facilities already in place. Traditional nursing homes can participate in culture change programs with great success if their leadership is committed to the philosophy through the transition period and beyond. They can retrain staff, add plants and pets and remove nursing stations, but the standard long hallways have remained – until now.
Last week I had the opportunity to speak with Rebecca Priest, LNHA, LMSW, Vice President of Skilled Services, at St. John’s Home in Rochester, NY. She’s presiding over one of the most exciting changes in LTC to come down the pike since, well, Green Houses.
St. John’s is taking a conventional nursing home built in the 1960’s with 32 beds to a hall and turning it into 22 small homes modeled after the Green House Project. Each floor is being systematically transformed into homelike environments with a large space for cooking, dining and socializing and universal workers called “Shahbazim” who are central to the model’s success.
Rather than having aides, housekeepers and laundry workers, the Shahbazim do it all. “The Shahbaz role,” Priest says, “is highly skilled and not for everyone. Shahbazim need to collaborate and be part of a highly sophisticated work team.”
Cross-training staff and flattening the work hierarchy reduces the likelihood that workers will find themselves in “systematically disempowered situations where they are set up to fail.” As a resident I knew used to say, “Amen to that!”
For the entire article, visit:
Home, small home





Interview with the Commissioner of the NYC Dept of Aging (Silo-Busting)
Here’s my latest article on McKnight’s Long-Term Care News:
Silo-busting
Ideas from an interview with Dr. Donna Corrado, Commissioner of the New York City Department for the Aging
Within long-term care, overcoming the problems caused by silos can lead to better care coordination, increased interdepartmental cooperation and reduced work redundancy.
My 1-on-1 interview with Donna Corrado, PhD, Commissioner of the New York City Department for the Aging, suggests there are also benefits to breaking down silos between public and private aging services.
Area Agencies on Aging (AAA)
There are 622 area groups in the National Association Area Agencies on Aging (n4a). According to its website, “the primary mission [of n4a] is to build the capacity of our members so they can help older adults and people with disabilities live with dignity and choices in their homes and communities for as long as possible.”
While n4a’s mission might seem diametrically opposed to the business interests of long-term care, this isn’t the case in a capitated model. When an organization offers a continuum of care with the goal of maintaining people outside of the hospital and at the least expensive level of care, then private and government (and personal) interests align.
My conversation with Dr. Corrado revealed ways of making the most of this alignment of interests, as well as ways to boost the census in long-term care.
AAA offerings
While NYC is the largest Area Agency on Aging in the country, each AAA has it’s own assortment of programs directed toward the needs of their community. There are core issues common everywhere.
Food insecurity is addressed through congregate meals in senior centers and through organizations like Citymeals on Wheels, which provides 8 million meals to New Yorkers Monday through Friday. At the National Readmission Prevention conference I wrote about last month, the speaker from Abbott Nutrition reported that proper nutrition resulted in a 28% decline in hospital readmissions over a six-month period.
Every community has a case management program that assesses individuals and offers home care services.
Senior centers (NYC has 270 of them!) can reduce the epidemic of loneliness and help identify health problems before they become medical emergencies. Funding for senior centers varies greatly, creating opportunities for collaboration.
For the entire article, visit:
Silo-busting


Readmission prevention: The role of post-acute providers
Here’s my latest article on McKnight’s Long-Term Care News:
Readmission prevention: The role of post-acute providers
Long-term care providers have an opportunity to thrive with value-based care, escape cynicism and join the growing wave successful at avoiding readmissions.
Last week, I was part of a panel discussing readmission prevention at the National Readmission Prevention Collaborative’s C-Suite Invitational: New York Transformational Healthcare, which focused on Accountable Care Organizations, bundles and readmissions. The goal of the forum was identifying ways for providers at all ends of the healthcare continuum to prevent hospital readmissions and to thrive in a value-based care model.
Unlike fee-for-service care, which compensates providers for each procedure, value-based care pays for the episode of care, making it essential to coordinate between providers and to avoid unnecessary medical utilization. Efforts to avert hospitalization and readmission are paramount.
The conference offered several takeaways for skilled nursing facilities and other post-acute providers.
From hospital to post-acute provider
Presenters emphasized the importance of being part of a continuing care network rather than a stand-alone facility and of working closely with referral sources. Because crucial information is easily lost during care transitions, best practices suggest a “warm handoff” rather than an exchange of information on paper or via computer, meaning that providers have an actual conversation about care.
To facilitate this, both the referral source, such as the hospital, and the accepting organization, such as the nursing home, should have someone to collect and relay information. To reduce costs, this needn’t be a clinical role as long as the necessary details are conveyed. Communication can be streamlined using a “hotline” between the hospital and the post-acute provider so that phone calls can be made directly rather than routing through the emergency department.
The transition to home
Hospitals are being monitored for readmissions and may have several post-acute care options. The facility most likely to prevent rehospitalization after discharging residents is the one most likely to get referrals.
For the entire article, visit:
Readmission prevention: The role of post-acute providers
![]()

How do they sleep at night?
Here’s my latest article on McKnight’s Long-Term Care News:
How do they sleep at night?
Perhaps you’ve heard about the administrator who spent a week as a resident in his long-term care facility. After being roused from sleep daily to receive medications that could have been dispensed later in the day, he banned his physicians from unnecessarily prescribing meds during night hours.
That’s an excellent way of attending to sleep hygiene, an important and often overlooked aspect of wellbeing for residents and staff alike.
Sleep challenges of older adults
By the time residents arrive at our doors, their sleep is likely to be affected by influences such as illness and pain. In addition, there are changes in circadian rhythms as people age, leading to increased wakefulness earlier in the morning and fatigue earlier in the evening, according to an article in this month’s American Psychological Association’s Monitor on Psychology.
While we can’t alter some of these factors, as care providers we can become more attuned to the importance of sleep for our residents and train our teams to create environments that are more conducive to slumber.
Impact on care
Poor sleep is associated with cognitive and physical deficits. It can impair residents’ ability to participate in rehab and negatively affect their moods and their interactions with others, including the staff members there to help them (whose job is hard enough).
Residents who can’t sleep through the night due to elements within the control of the facility are not happy with this situation. They’re less satisfied with their stays and therefore less likely to recommend the facility to their friends and neighbors.
As illuminating as it would be, you needn’t sleep in your facility for a week to find out which staff training and policies will remedy the problem. The residents have told me what keeps them up at night and I’ve outlined a “sleep hygiene” training program based on that.
For the entire article, visit:
How do they sleep at night?