Category: McKnight’s Long-Term Care News
Posted by Dr. El - March 19, 2018 - Books/media of note, Business Strategies, McKnight's Long-Term Care News

Here’s my latest article on McKnight’s Long-Term Care News:

Three new books on aging and healthcare recently crossed my desk, each with completely different takes on our industry.
One focuses on ways in which companies, including long-term care organizations, can save on healthcare costs. In another, the author’s insights into elder wisdom can be used by facilities to add to the quality of life of residents. The final book offers an outsider’s view into how our field is perceived by older adults and their families.
Cost savings
In “Health-Wealth: 9 Steps to Financial Recovery,” author Josh Luke, Ph.D., a former hospital CEO turned “healthcare futurist,” argues that our healthcare delivery system is so badly broken that we should seek a new model for the healthcare needs of employees.
He outlines a method to implement a consumer-driven model that improves pricing transparency and control over costs. Some of the suggestions are likely to both reduce expenses and increase employee satisfaction. For example, an organization-wide emphasis on health and wellness can be a popular program with medical savings.
Other ideas, such as charging the employee a percentage of care costs over their maximum deductible, won’t be universally appealing but could influence workers to choose more affordable “centers of value” during a health crisis.
If organizations find creative ways to reduce healthcare expenditures for their employees, the market is bound to shift in unexpected directions — and that’s exactly what “industry disruptor” Josh Luke is hoping for.
Quality of life
The second book, “The End of Old Age” by Marc Agronin, M.D., offers a hopeful view of aging that will resonate with those in the field.
I was particularly struck by the fact that Agronin, a geriatric psychiatrist, began his book with a chapter on why we should grow old, addressing issues around end of life choices and the way we approach old age. The foundation of acknowledging that some people don’t actually want to live to old age is a crucial exploration that sets the tone for the rest of the book.
Subsequent chapters point to the value of aging in very specific ways. While older adults may not surpass younger people at tasks that require speed or visual acuity, for example, Agronin details five different forms of wisdom in which elders excel. The book includes tools so that others, such as families and staff members, can use his model to help elders make use of their strengths and recognize their purpose at this phase of life.
For the entire article, visit:



Posted by Dr. El - March 9, 2018 - Books/media of note, Business Strategies, McKnight's Long-Term Care News

McKnight’s Online Expo, FREE, March 14th and 15th 2018
Earn 5 Free CEUs at 5 Free webinars

Once again, McKnight’s will host its annual online expo, which is a chance to attend a conference without leaving your desk. Register for the conference in advance, and then log in to hear the talks, visit the vendors, and chat with the reps and attendees.
This year’s topics are:
PAYMENT: Operational strategies for surviving regulatory, payment and database changes
WOUND CARE: Is the Braden Scale increasing your facility’s risk of malpractice?
TECHNOLOGY: Telehealth and Reimbursement: What you need to know for the near term
QUALITY: Beyond a fire drill: Emergency prep steps for active shooters in your building
CAPITAL: The new funding sources
Posted by Dr. El - March 3, 2018 - Business Strategies, Communication, McKnight's Long-Term Care News, Motivating staff

Here’s my latest article on McKnight’s Long-Term Care News:

When we think of teamwork in long-term care, we envision a group of dedicated specialists working together to provide the best care for our residents. They read notes from other disciplines, bounce ideas off colleagues at the nursing station and convene care plan meetings.
In reality, teamwork in long-term care is much more complex.
Teamwork basics
Team members include not just clinical staff, residents and family members, but other workers who frequently have an influence on care, including housekeepers, laundry workers, maintenance staff and security guards. To enhance teamwork, these employees should be included in in-service trainings that might initially appear beyond their purview, such as customer service training and education about the medical and behavioral information they may need to relay to the nurses.
Teamwork is strengthened when team members understand the work of their colleagues and when it can best be utilized. For example, a lack of understanding of the difference between psychology and psychiatry services can cause delays in the receipt of needed treatment. Consider monthly training lunches that can boost morale, increase interdepartmental understanding and improve team functioning.
Team members also include those outside the facility, such as medical specialists, dialysis centers and hospitals, as well as consultants who provide onsite care such as psychiatrists, dentists, respiratory therapists and others.
Unifying all these team members requires uncomplicated and reliable conversation and correspondence. Communication can be enhanced in a variety of ways, including computerized records that eliminate paper consults and indecipherable handwriting, enhanced change of shift reports that include behavioral as well as physical information and a management commitment to staff retention to create the stability necessary for a solid team.
Taking it further
Once teamwork basics of role understanding, stable staffing and communication are covered, teams can begin to address teamwork at a deeper level.
Deep teamwork involves observing how the floor, unit or neighborhood is functioning as a whole over different shifts.
A team is not functioning well if a disruptive resident is keeping others awake at night or frightened during the day. Nor is it a high functioning team if two staff members are in a personal argument that’s obvious to all who walk onto the floor.
Deep teamwork calls for observing the interactions of the team and intervening as necessary to guide them back on track.
For the entire article, visit:

Posted by Dr. El - February 15, 2018 - Business Strategies, Customer service, Inspiration, McKnight's Long-Term Care News, Resident care, Tips for gifts, visits

Here’s my latest article on McKnight’s Long-Term Care News:

Last week, I attended an accessible design symposium at the Cooper Hewitt Museum in New York City to see what ideas I could use with elders in long-term care. Through listening to the symposium speakers, reading descriptions of works featured in the student design contest and viewing the Access+Ability exhibit, I found more than I had expected.
Crash course in accessible design
I suspect I’m not the only McKnight’s reader with a lack of knowledge about accessible design — even though we work with elders with abilities that are typically different than those of younger adults.
Patricia Moore, introduced as “the mother of universal design,” told the audience that her elderly grandparents inspired her work. They struggled to maintain their independence in a world that made it difficult for them. “Grandma wasn’t broken,” she said. “The tools we gave her were inadequate.”
In my crash course in accessibility, I learned that objects can be designed in ways that increase the mismatch between our bodies and the environment or, in accessible design, to intentionally decrease that mismatch. For example, the standard design of a walking cane allows it to fall to the floor, making it difficult to retrieve for someone with mobility problems. In the Cooper Hewitt exhibit, I saw canes that stayed upright when not in use.
Another speaker discussed how “designing for disability” very often results in products that are good for everyone, such as books on tape, height adjustable desks or ramps for building access that are used by parents pushing strollers and travelers with rolling suitcases, in addition to those with walkers or wheelchairs.
Nothing about us without us
There was a small, vocal group of disability activists present. When I entered the symposium I was handed a card from their organization that read, “Nothing about us … without us.” They echoed the sentiment of the speakers that increasing the diversity of people designing products and systems results in products and systems that work better for a larger number of people.
Including elders and direct care staff in more of the decisions that affect them within our organizations is likely to result in better decisions.
For the entire article, visit:

Jeweled Hearing Aids

Posted by Dr. El - January 31, 2018 - Business Strategies, McKnight's Long-Term Care News, Resident education/Support groups, Transitions in care

Here’s my latest article on McKnight’s Long-Term Care News:

Amy Gotwals, the Chief of Public Policy and External Affairs at the National Association of Area Agencies on Aging, kicked off the 28th Annual Aging Conference in New York City last week, held at the New York Academy of Medicine and filled with attendees providing community-based care for elders. Her rousing keynote outlined the vast care demands of the growing wave of elders and the importance of building healthcare partnerships.
Some of Gotwals’ statistics were startling despite knowledge of the impending “silver tsunami.” Some areas of the country are projected to see an increase in Alzheimer’s diagnoses of 50% to 80% by 2025. Family caregivers between 65 and 74 years old provide more than 30 hours of care per week; for those 75 and older, it’s more than 34 hours each week.
Statistics such as these point to ways in which long-term care organizations can position themselves to be relevant far into the future by offering, for instance, memory or respite care.
Gotwals reported that local Area Agencies on Aging (AAAs), of which there are 622 across the country, are increasingly contracting with healthcare organizations to provide services such as care transitions, nutritional services, home evaluations and evidence-based self-management for chronic diseases.
In one example, San Francisco’s Institute on Aging (IOA) partnered with a nonprofit, community-based housing agency and contracted with the Health Plan of San Mateo County to provide care management services that reduced monthly spending per member by nearly 50%.
While local organizations may not be as seasoned in business promotion, they’re experts in the needs of the local community and their established presence in the neighborhood can be a boon to long-term care organizations seeking to create new partnerships.
ElderTech
After hearing Gotwals’ opening remarks, I chose a breakout session on technology and design presented by Tom Kamber, Ph.D., founder and director of Older Adults Technology Services (OATS). His is a national organization that provides technology-based senior centers and collaborates with a wide range of institutions to address the tech needs of elders.

Posted by Dr. El - January 18, 2018 - Communication, Customer service, McKnight's Long-Term Care News

Here’s my latest article on McKnight’s Long-Term Care News:

As “Eileen” suggested in the comments section of a recent “Dr. El” blog, disclosing personal information can be a good way to establish a more intimate connection with residents. While self-disclosure can create warmer relationships, there also can be unintended and unwanted consequences to revealing such details.
In contrast to psychologists who study interpersonal interactions for a living, staff members are unlikely to have fully considered the impact of their self-disclosures. Doing so can improve their relationships with residents and avoid unanticipated pitfalls.
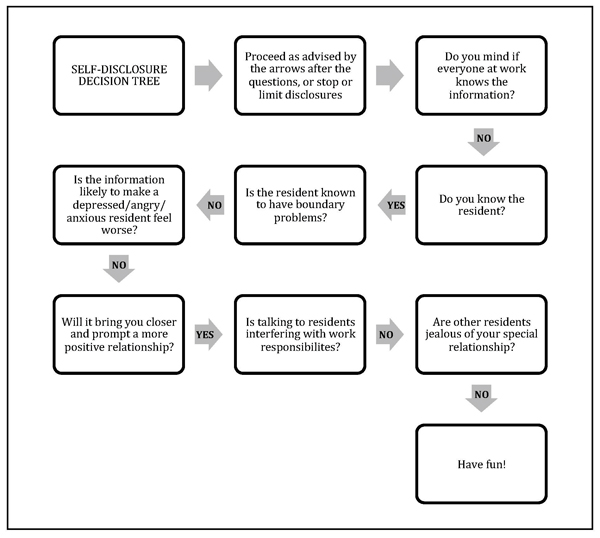
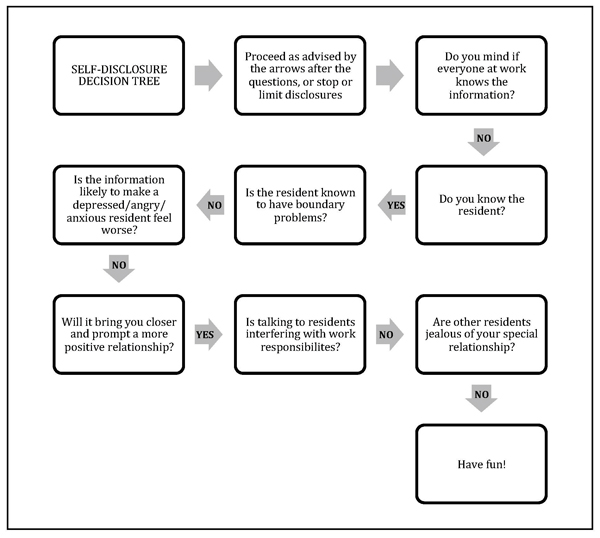
Here’s a guide* to the ups and downs of self-disclosure along with a handy flow chart (see below) to help you and your team decide when it’s the right move in any given situation. My inclination toward privacy is reflected in the flow chart, so consider it a starting point for discussion among team members or in a staff training session.
The ups
Part of the pleasure in working with elders is hearing about their lives and learning from their experiences. Sometimes revealing a detail or two from our own lives can help a reticent resident open up.
Self-disclosure allows workers to be more open and relaxed at work and to establish deeper relationships with those in their care.
Being “real” with residents can reduce the somewhat artificial boundaries between people in different phases and roles in their lives and can be part of a healthy organizational culture.
The downs
On the other hand, self-disclosure can sometimes get workers in trouble.
For the entire article, visit:
Posted by Dr. El - January 4, 2018 - Business Strategies, Communication, McKnight's Long-Term Care News, Motivating staff

Here’s my latest article on McKnight’s Long-Term Care News:

Ahhh. A new year. It’s time for a fresh start, the chance to take life in a different direction.
Many of my friends have remarked to me that they want more focus on family and friends this year. They’d like to achieve a better balance between work and home.
On the job in long-term care, perhaps the goal is to tackle the staff turnover problem or increase profitability. Or maybe the hope is that resident, staff and family satisfaction ratings will be better in 2018 or that this might be the year to achieve a five-star rating.
The common thread between these goals is deepening the attention paid to the people in our personal and business lives.
When staff members don’t feel valued, or inspired by the mission of the company, turnover increases, making it virtually impossible to have high satisfaction scores and five-star ratings. Repeatedly recruiting and training new staff cuts into profit margins and damages worker morale.
To turn things around in one’s personal life, conscious decisions can be made around limiting time on electronics or choosing to fill the new calendar year with events that connect loved ones. At work, changes can occur by prioritizing the way staff members are treated and revamping the culture of the company, altering the way people interact.
Whatever our roles in LTC, there are steps each of us can take to enhance the way we treat each other and to have a positive impact on workplace culture.
• Reevaluate mission and culture. Readers in a position to revise the organizational customs as a whole might enlist experienced guides in the process. A consulting and coaching company such as Drive, with which I’m affiliated, evaluates the strengths and weaknesses of a healthcare organization and provides ongoing support to meet goals throughout the culture change process. As a Drive team member notes in this article onCreating and Sustaining a Strong Culture, follow-through is essential. A consulting team can ensure that bumps in the road don’t become dead ends.
• Investigate known culture change programs. Thankfully, there are many people in our field who have undertaken the daunting task of creating a more gratifying long-term care environment while still following regulations. The new year is an excellent time to take a class with the Pioneer Network or the Eden Alternative, or to learn more about The Green House Model at their 1/9 webinar.
• Promote kindness. If your job in long-term care doesn’t allow you the opportunity to change the overall organizational framework, you can still be an important influence on others with whom you interact by focusing on kindness.

Posted by Dr. El - December 21, 2017 - For Fun, Inspiration, McKnight's Long-Term Care News, Personal Reflections, Something Good About Nursing Homes

Here’s my latest article on McKnight’s Long-Term Care News:

From the 102-year-old Hulk Hogan fan to the doting, selfless caregivers doing behind-the-scenes work, there are numerous people in long-term care who inspired me this year.
Take, for example:
• The 102-year-old man, still remarkably handsome, whose favorite sport is professional wrestling and who recalls fondly the days of Hulk Hogan.
• The personal companion I encountered dusting the framed family photos on the windowsill while the blind woman she cared for was taking a nap.
• The new assistant administrator who stopped me in the hallway to introduce himself and who seemed genuinely interested in my response.
• The nurses who immediately come up with a solution to a resident’s problem and then follow through with it. (“If he wants to be down at rehab early, we’ll have the night shift get him up before they leave.”) Hallelujah!
• The housekeeper dedicated to controlling infection even though it’s been a tough year for her personally.
• The legally blind 90-year-old woman who avidly follows the news and the music scene and has a strong opinion on everything. That Gaga is great, she says. The president is not.

Posted by Dr. El - December 7, 2017 - Anecdotes, End of life, McKnight's Long-Term Care News, Personal Reflections

Here’s my latest article on McKnight’s Long-Term Care News:

I lost one of my two mothers-in-law last Monday, five weeks after she was diagnosed with pancreatic cancer. We had expected Audrey to reach 100 years of age, like her mother, but she died shortly after her 91st birthday, having spent her 90th year traveling and doing water aerobics three times a week.
Audrey had filled a hole in my life left after the death of my beloved great-aunt many years ago. Whenever I phoned my MIL, she’d answered the phone with a chipper, “Oh hello, Darling!” Emails began with the salutation, “Dear Heart,” before launching into the latest goings-on at the CCRC where she was the head of several resident programs.
After her diagnosis, she enlisted peers to take over her responsibilities, giving them her notes and training them as if they were new employees. She considered beginning a program at the care center during her brief stay, “Can you believe they don’t recycle here? I’m going to make some calls and see if we can get that started.”
She spent her last weeks shipping sentimental items to various relatives and, when she became too weak, she began instructing her sons to do the same. A steady stream of family members and friends came to say goodbye to her as she sat in her bedside chair with her makeup on and a scarf neatly tied around her neck.
It was exactly the way I’d want to go if I could have my choice.
In the days after she died, I phoned her sons and notified family members on our side of the family. I called a few of my friends and tried to get extra sleep. I confirmed my parents’ upcoming lunch invitation. I spent quality time with the cat, and with my family. I ate some chocolate.
For the entire article, visit: Elder love

Posted by Dr. El - November 22, 2017 - Business Strategies, Customer service, McKnight's Long-Term Care News, Motivating staff, Resident care, Something Good About Nursing Homes

Here’s my latest article on McKnight’s Long-Term Care News:

In 2014, I wrote, “I finally visit a Green House (and it blows my mind).” The Green House is designed with a spacious common area, private bedrooms and showers, unobtrusive medical items and universal workers practicing person-centered care. The model shows that it’s possible to make dramatic lifestyle improvements in long-term care.
It seemed that Green Houses were the answer, if only there weren’t so many traditional facilities already in place. Traditional nursing homes can participate in culture change programs with great success if their leadership is committed to the philosophy through the transition period and beyond. They can retrain staff, add plants and pets and remove nursing stations, but the standard long hallways have remained – until now.
Last week I had the opportunity to speak with Rebecca Priest, LNHA, LMSW, Vice President of Skilled Services, at St. John’s Home in Rochester, NY. She’s presiding over one of the most exciting changes in LTC to come down the pike since, well, Green Houses.
St. John’s is taking a conventional nursing home built in the 1960’s with 32 beds to a hall and turning it into 22 small homes modeled after the Green House Project. Each floor is being systematically transformed into homelike environments with a large space for cooking, dining and socializing and universal workers called “Shahbazim” who are central to the model’s success.
Rather than having aides, housekeepers and laundry workers, the Shahbazim do it all. “The Shahbaz role,” Priest says, “is highly skilled and not for everyone. Shahbazim need to collaborate and be part of a highly sophisticated work team.”
Cross-training staff and flattening the work hierarchy reduces the likelihood that workers will find themselves in “systematically disempowered situations where they are set up to fail.” As a resident I knew used to say, “Amen to that!”