Category: Resident care
Posted by Dr. El - February 16, 2016 - Business Strategies, Communication, Customer service, McKnight's Long-Term Care News, Resident care, Technology

Here’s my latest article on McKnight’s Long-Term Care News:

In “A potential lawsuit in every worker’s pockets?”, McKnight’s Editorial Director John O’Connor describes two of many recent incidents of long-term care workers using their cell phones to record residents in embarrassing situations and post the photo or video to social media.
Despite leading to termination of employment and lawsuits, some of the employees involved appear to have no idea that this behavior is a serious ethical breach. Staff writer Emily Mongan offers the following quote in her article on this topic: “They just blew everything out of proportion,” [the offending employee] said. “It was just a picture of her butt.”
Wondering how an employee could possibly think posting a photo of a resident’s behind to social media would be a reasonable action to take, I contacted psychologist and social media expert Keely Kolmes, PsyD , to find out.
Changing expectations of privacy
Dr. Kolmes notes that it’s become commonplace for people to record moments from their lives and post them to social media, generally without consent from others who might be captured in the photos or videos that are shared.
For example, while I get my daughter’s permission before I post anything about her to my private Facebook page, I occasionally find her featured in photos with friends on their pages without prior approval. Posting friendly pictures is considered acceptable in one’s personal life (and a parent who asks permission from their child is, I suspect, unusual).
One might argue that there’s a distinction between personal and professional situations, yet similar situations frequently occur in professional settings as well, such as discovering you’ve been featured in a photo on the website of an organization after attending their conference or on your facility website after the holiday party.
Most people are pleased to be highlighted in such photos, but if an organization expects employees to follow their social media policy, these situations are a prime opportunity to show workers that the policy is being followed at the corporate level as well. At facility events, for instance, notify staff members that photos will be taken and may be posted.
Resident/staff boundaries: Whose life/home is it?
For the entire article, visit:

Posted by Dr. El - November 12, 2015 - Business Strategies, Customer service, Dementia, End of life, McKnight's Long-Term Care News, Medication issues, Motivating staff, Resident care

Here’s my latest article on McKnight’s Long-Term Care News:

Despite the diversity of the events I attended during my brief visit to the LeadingAge convention in Boston last week, a theme clearly emerged. The thread that ran through the varied offerings was well-being.
Retaining staff
In researcher and consultant Joanne L. Smikle, PhD’s talk on staff retention, rather than focusing on why employees are leaving, she looked instead at why they stay.
Based on her studies of long-term care organizations, she found that “if the leadership of the organization lacks passion, you will have trouble with retention and commitment.”
In healthy organizations, staff members “from the top of the house to the bottom of the house” stay because they can say, “I felt I mattered.” Experiences that contribute to that feeling: Recognizing staff in formal and informal ways, an open dialogue with staff rather than top-down communication, and a focus on the human elements enabling employees to make connections with each other, the residents and the families.
Dementia care
G. Allen Power, MD, FACP titled his presentation, “Enhancing well-being for people living with dementia,” so it wasn’t surprising that this was a central point in his talk.
He asserted that antipsychotics don’t work and don’t treat the true causes of the behaviors associated with dementia. Instead, he recommends focusing on the seven primary domains of well-being, which are part of the Eden Alternative model of care: identity, growth, autonomy, security, connectedness, meaning and joy.
In one instance, a resident who became agitated when he was prevented from leaving the building was allowed outside. The man looked at the cows in a nearby field and returned to spend the rest of the day calmly. The team, who subsequently learned that the resident had been a farmer whose daily routine included an early morning check on his animals, had given him not only autonomy, but had also affirmed his identity and added meaning and joy to his life. His agitation disappeared.
Keynote address
Atul Gawande, MD delivered a Monday morning keynote address. Author of the book “Being Mortal,” Dr. Gawande discussed ways in which to improve end of life treatment. He advocated for care that takes into account the desires of the patient and noted that there is more to living than extending the amount of time we live.
For the entire article, visit:

Leonard Florence ALS unit entrance
Posted by Dr. El - October 8, 2015 - Communication, Customer service, Resident care

New York Times writer Jane Brody recently penned two excellent columns on the value of hearing aids and the obstacles to obtaining them. (The links to these articles are below.) The articles led me to reflect on my experience with hearing aids as a psychologist in long-term care. I’ve noticed additional obstacles to hearing aid use:
- The aids are in the dresser drawer rather than the ears of the residents who need them.
- The hearing device is locked in the nursing cart or closet.
- The batteries are no longer functioning and there are no backup batteries.
Here are some suggestions to remedy these challenges:
- Nurses, aides, ombudsmen, readers: Please consider putting in hearing aids as essential a part of getting ready for the day as putting on a shirt.
- Establish a convenient location for all assistive devices so that eyeglasses, hearing aids, and dentures are easy to find and store. A special caddy for a dresser drawer would be very helpful in keeping track of these important items.
- Keep backup batteries available so that dead batteries don’t mean several weeks of isolation. Sell batteries on an Independence Cart, or traveling store.
As Jane Brody points out in her articles, losing the ability to hear can lead to social isolation, cognitive impairment, excessive fatigue and other maladies. Let’s do what we can to keep our residents at their best.

Posted by Dr. El - September 25, 2015 - End of life, Resident care

In Paula Span’s column today in the New York Times’ New Old Age column, Near the End, It’s Best to Be ‘Friended’, she discusses the increasingly common situation of elders who have no representatives assigned to make healthcare decisions on their behalf.
She encourages seniors to dig deep into their social networks to find an appropriate candidate to become a healthcare proxy or to keep detailed directives in a location that’s accessible to healthcare providers.
Span notes state efforts to increase the number of people who can step into such a role — some states allow for a “close friend” or a niece, nephew or grandchild to become a medical decision-maker.
Healthcare organizations such as the Cleveland Clinic have created protocols to assist teams in medical decision-making for “unbefriended” elders who are without the capacity to express their own wishes. As the medical decisions become more serious — such as a surgery or a do-not-resuscitate order — two medical professionals and an ethicist must agree that the procedure is in the patient’s best interest. Withdrawing treatment requires two physicians and the approval of a subcommittee of the hospital ethics committee.
Long-term care facilities would benefit from establishing similar protocols and committees for what will undoubtedly become a more frequent circumstance as baby boomers — who are less often married and more often geographically isolated from relatives — enter our care in greater numbers.
For Paula Span’s article, visit: Near the End, It’s Best to Be ‘Friended’

Posted by Dr. El - August 18, 2015 - Inspiration, McKnight's Long-Term Care News, Personal Reflections, Resident care, Role of psychologists

Here’s my latest article on McKnight’s Long-Term Care News:

Last week, a New York Times article referred to the lack of training to prepare doctors to recognize the spiritual needs of their patients. Hospital physician Robert Klitzman, M.D., emphasized in the Well section article the value of meeting these needs.
Psychology graduate school also avoided focusing on clients’ spiritual needs, which were considered to be the province of those with formal religious training. Despite this, I’ve found that many of the conversations I have with residents can be considered spiritual work.
In the beginning of my LTC career, I quickly recognized that in order to be of service in this environment, I needed to come to a spiritual understanding of how such nice people could be dealing with such difficult illnesses. This led me to the book by Harold S. Kushner, “When Bad Things Happen to Good People.” The gist of the book, as I recall it, was that the question is not so much, “Why me, God?” but, “Why not me?”
That stance allows me to help people come to terms with their experiences and also to recognize very clearly that this could be me, or me down the road a few paces. I am merely assisting others as I hope someone will assist me when it’s my turn.
For the entire article, visit:

Posted by Dr. El - July 2, 2015 - Communication, End of life, Engaging with families, Resident care

Here’s an important article in the New York Times Opinionator Column by Ellen Goodman, one of the founders of The Conversation Project (which I’m about to investigate further). Note her comment that she expected her mother’s doctors to tell her what to do. The families of our residents are expecting the same from us.
I was 25 when I flew home for my father’s last birthday. His cancer had returned and he would die three months later at the age of 57. What I remember most about that weekend was the large rectangular gift box he opened. My mother had bought him a new suitcase.
I don’t know if that suitcase qualifies my family for the Denial Hall of Fame. There are so many contenders for that honor. But I’ve carried the psychic baggage over the years. I have never forgotten that image and how we lost a chance to say goodbye. I still wonder if my father was lonely in the silence that surrounded our inability to talk about what we all knew.
Decades later my mother began a long slow decline. By then, I was a newspaper columnist, a job that I often described as “telling people what you think.” I was professionally outspoken. But little had changed since my father’s death.
Yes, my mother and I talked about everything — but we didn’t talk about how she wanted to live toward the end. The closest we ever came to discussing her wishes was when she would see someone in dire straits and say, “If I’m ever like that, pull the plug.” But most of the time there is no plug to pull.
Gradually and painfully, my mother lost what the doctors call “executive function,” as if she were a C.E.O. fumbling with Excel spreadsheets, not a 92-year-old who couldn’t turn on the television or make a phone call. Eventually, she couldn’t decide what she wanted for lunch, let alone for medical care.
In some recess of my mind, I still assumed that death came in the way we used to think of as “natural.” I thought that doctors were the ones who would tell us what needed to be done. I was strangely unprepared, blindsided by the cascading number of decisions that fell to me in her last years.
For the rest of the article, visit:

Posted by Dr. El - June 24, 2015 - Business Strategies, Communication, McKnight's Long-Term Care News, Resident care

Here’s my latest article on McKnight’s Long-Term Care News:

An experienced colleague was recently let go from her job to which she’d been dedicated for 10 years. “We want to take things in a different direction,” she was told by the administrator. “Pack up your office and go.”
An hour later, she was in the parking lot holding a box containing a photo of her kids and mementoes of a decade as head of the social service department. Her replacement started two days later.
There are, of course, occasions when people who are fired or otherwise are terminating employment and need to be escorted from the building. But many workers are career professionals who wouldn’t consider burning bridges with bad behavior. Despite this, I’ve witnessed hasty dismissals and hushed resignations on multiple occasions throughout my career.
Sometimes, departing coworkers will tell me they didn’t want to let anyone know they were leaving because they didn’t want to deal with the residents’ being upset.
In my training to become a psychologist, we spent a great deal of time discussing endings and termination of treatment. While work in long-term care isn’t necessarily a psychotherapeutic relationship, I believe leave-takings in LTC are more important than in other settings and that the style of departure should be given more consideration.
Here are some aspects to consider:
• Due to the nature of the work, staff members form deep relationships over time with the residents and their families. When we depart, it matters to them.
• Because we work with elders and those who are ill, people are constantly leaving — through death, discharges, and hospital transfers — often suddenly and without the chance to say goodbye. This can create small traumas. In compassionately addressing our departures, we have the opportunity to reduce the amount of trauma in the lives of our residents rather than contribute to it.
For the entire article, visit:

Posted by Dr. El - May 27, 2015 - Dementia, Engaging with families, McKnight's Long-Term Care News, Resident care, Role of psychologists

Here’s my latest article on McKnight’s Long-Term Care News:

A recent Iowa court case acquitted Henry Rayhons of sexually abusing his wife, who had Alzheimer’s dementia and lived in a nursing home. The case not only prompted national debate, it led those in long-term care to consider how to handle sexual activity within the bounds of their facility, particularly in cases when one or both of the parties have a diagnosis of dementia.
Psychologists are frequently asked to determine whether or not a patient has the capacity to understand or authorize various aspects of care, including their ability to consent to sexual behavior.
Eric Redlener, PhD, president of The PsychAssociates Group, a company that provides psychological services to long-term care facilities, held a meeting for its supervisors to discuss the challenges that arise when considering capacity, sexual activity and the senior living environment.
I was on the conference call since I work for them regularly. Here is a fly-on-the-wall account of the concerns raised during the meeting.
Staff issues
Some of the challenges to handling sexual behavior in the long-term care environment involve the reactions of staff members to the situation.
· Some staff members show squeamishness about “Grandma and Grandpa” having sex.
· Staff members may be concerned, rightly or wrongly, that residents will be taken advantage of.
· Staff members project their notion of sex onto elders. Elders may be content with holding hands or heavy petting, but staff might be anticipating people “swinging from the rafters.”
· Sometimes an administrator or director of nursing bans sexual activity among the residents, considering it “bad behavior,” despite the fact that it’s a legal right in many states for residents to be able to engage in sexual relations within a long-term care facility.
Family concerns
The reaction of family members to the romantic/sexual involvement of their elders can vary greatly.
· Some family members are able to accept their loved one’s need for intimacy, despite its sometimes unexpected expression, such as when an elderly heterosexual mother spends time cuddling with another woman on the floor, or a husband with dementia becomes involved with a woman who is not his wife.
For the entire article, visit:

Posted by Dr. El - May 13, 2015 - Bullying/Senior bullying, Dementia, McKnight's Long-Term Care News, Resident care, Something Good About Nursing Homes
Here’s my latest article on McKnight’s Long-Term Care News:

I’ve been fortunate enough to attend several senior living conventions recently and my enthusiasm for the experience has yet to diminish. If you haven’t yet had the opportunity to be present for a conference (or if it’s been a while since your last one), consider these reasons for attending:
• There are interesting discussions that directly relate to day-to-day work. Hearing different ideas and perspectives can offer a new way to handle problems and can help you get out of a work rut.
• The conference discourse provides a great opportunity to brainstorm, on your own or with colleagues and coworkers.
• Attendees are often equally enthusiastic about LTC and the connections made with others there can help implement changes within your organization.
• The new products offered in the expo hall can improve operations and the lives of residents and staff.
• Sharing the lessons learned with coworkers can expand the value of the conference.
If an onsite convention isn’t possible for now, consider attending a virtual event, such as the annual McKnight’s Online Expo, which not only offers educational sessions but also has chat rooms and a virtual expo hall.
My experience at ALFA
My most recent conference was the Assisted Living Federation of America convention last week in Tampa, where I spoke at the session “The Importance of Environmental Factors in Senior Living.” During my whirlwind visit to ALFA, I was also able to take in two presentations and spend time in the expo hall.
One of the sessions was on using recreational activities as a way to improve morale among residents and staff and to promote your organization in the community. I’ve spoken about these goals in my audio, “10 Steps to Making Recreation the Most Valuable Department in the Nursing Home,” and I was encouraged to hear of unique ways senior organizations have been serving these dual objectives, such as knitting caps for premature babies.
The conversation among participants helped me think about the impact that the pro-social engagement of residents has on reducing the problem of senior bullying. If seniors are busy doing good in the world, not only are they less likely to be engaging in negative behavior such as bullying, but the organization has helped to create a culture of caring.
The second talk was a roundtable on engaging staff in order to reduce turnover. The suggestions focused on hiring for attitude and training for skills, being clear about the mission of the organization, and implementing programs that reward employees for their good work.
Expo hall jewels
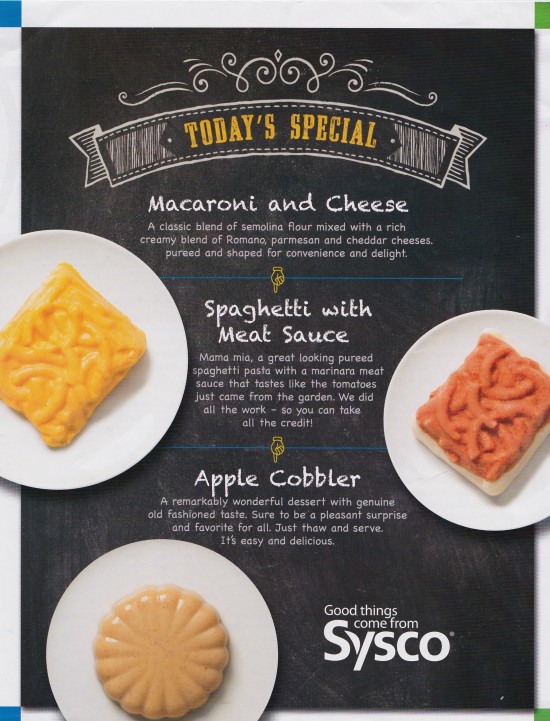
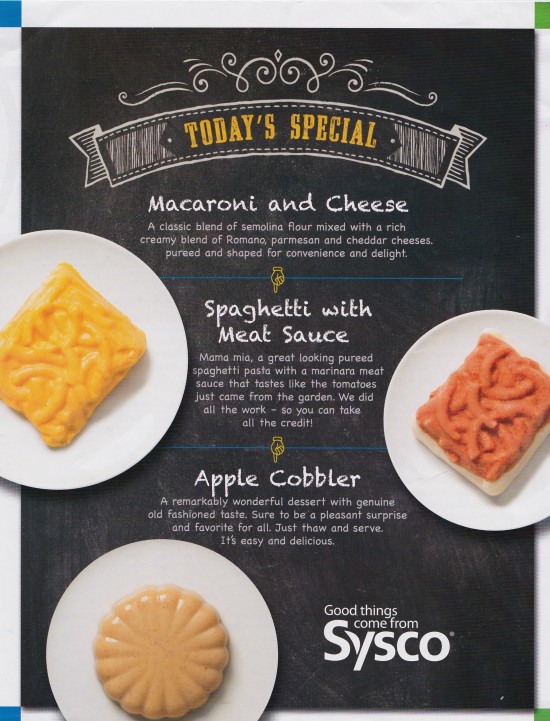
As usual, I searched the expo hall to find products I knew my residents would appreciate.
Having heard far too many elders complain bitterly about pureed food, I was delighted to find a company that offered puree solidified into colorful, shaped molds that were far more appetizing than typical puree. The saleslady looked askance at my glee about getting to sample her wares — but regular readers know I like to experience things from the residents’ perspective whenever possible.
For the entire article, visit:

Posted by Dr. El - April 15, 2015 - Depression/Mental illness/Substance Abuse, McKnight's Long-Term Care News, Resident care

Here’s my latest article on McKnight’s Long-Term Care News:

The elevator opened up to the third floor of the skilled nursing facility. Wheelchair-bound residents lined the hall across from the nursing station, some silently watching the staff, some snoozing.
On the second floor of the nursing home, the physical layout was exactly the same but the atmosphere was completely different. Groups of two or three residents were chatting animatedly, commenting wryly on their observations of staff and laughing amongst themselves.
How do we get from Scenario A to Scenario B more often? Is it worth the effort?
The high cost of loneliness
A recent study showed that community-dwelling seniors visited their doctors more often when they were lonely — the trips to medical offices were an important but costly form of social interaction. Similarly, one might speculate that socially isolated residents request help from their nurses, aides and other workers due to feelings of loneliness in addition to addressing specific care needs.
Reducing loneliness among residents would, therefore, contribute to more staff time being available for medically necessary care.
Decreased turnover
The findings from another study suggest a connection between happier residents and staff retention. Researcher Barbara Parker-Bell, PsyD, LPC, ATR-BC, finds that “nurses consistently described the best and most satisfying aspects of dementia care as … the pleasure of seeing residents calm and engaged.”
I know from my own experience that it’s much more uplifting to step onto a unit with laughter than it is to work on a floor where the residents are depressed, lonely and withdrawn. And, of course, it’s better for the residents and their families.
Beyond ‘recreation’
Good therapeutic recreation programs are essential in reducing isolation, providing meaningful ways of spending time and in developing friendships. They’re an important step in reducing loneliness, but are also only one piece of the puzzle.
If all staff members consider the social aspects of the environment — one of the best selling features of life in LTC — we can create friendly, engaging interactions that build upon and extend formal recreation programs.
Challenges to interacting
For the entire article, visit: